Abstract
Chronic pain occurs in about 40% of individuals with sickle cell disease (SCD) and can significantly impair patient functioning. Neuropathic pain, defined as pain initiated by dysfunction of the peripheral and/or central nervous system, also plays a role in SCD pain. Despite this knowledge, there are minimal data evaluating patient reported outcomes (PROs) for individuals with SCD who have chronic pain. Further, data supporting the contribution of the neuropathic component to chronic pain in SCD are not well described. The objective of this study was to compare PROs between individuals with SCD who have chronic pain and those who do not. We hypothesized that PROs in individuals with SCD who have chronic pain will indicate worse patient functioning and those with chronic pain will have a more neuropathic component compared to individuals without chronic pain.
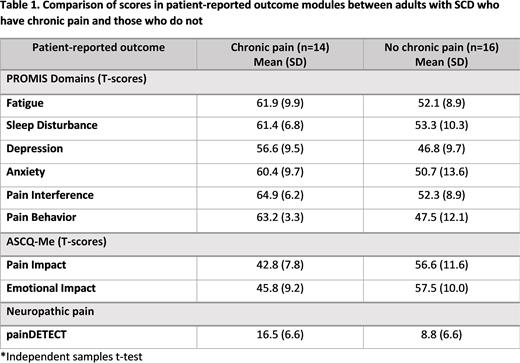
Individuals ≥18 years with SCD were eligible for inclusion. Individuals reported the number of days of pain in the past month and were considered to have chronic pain if they had pain every day, 5-6 times a week, 3-4 times a week or more than 10 times a month for at least the past 6 months. We based these diagnostic criteria on those defined by the America Pain Society Pain Taxonomy Initiative for chronic SCD pain. Individuals were assessed during their baseline state of health. All individuals completed Patient Reported Outcomes Measurement Information System (PROMIS) PROs including domains of Fatigue, Sleep Disturbance, Depression, Anxiety, Pain Interference, Pain Behavior; the Adult Sickle Cell Quality of Life Measurement Information System (ASCQ-Me) including domains of Pain Impact and Emotional Impact; and the neuropathic pain screening tool, painDETECT questionnaire. PROMIS and ASCQ-Me scoring uses a T-score metric where 50 is the mean of a relevant reference population and 10 is the standard deviation (SD) of that population. Higher T-scores for PROMIS modules indicate more of the concept being measured (e.g. higher T-score for the domain of Pain Interference indicates higher interference due to pain). On the contrary, higher ASCQ-Me T-Scores for the Emotional and Pain Impact domains indicate better self-reported health. painDETECT scores range from -1 to 38 with higher score indicating increased probability of neuropathic pain. Further, scores 19-38 indicate a definite neuropathic pain component, 13-18 indicate a probable neuropathic pain component, and 0-12 indicate a neuropathic pain component does not exist. We compared PROMIS and ASCQ-Me domain T-scores and painDETECT scores between individuals who have chronic pain and those who do not using independent samples students t-test. A p-value of <0.05 was considered significant.
A total of 30 adults living with SCD were enrolled. The mean age of our sample population was 33.9 (SD 10.2) years with range of 19-58 years and 43.3% (n=13) were female. We found 46.7% (n=14) of the study cohort had chronic pain. There were no significant differences in sex or age between those who do and do not have chronic pain. Table 1 displays the PROMIS, ASCQ-Me, and painDETECT scores in those that do and do not have chronic pain and the differences in scores between the two groups. All PROMIS scores in individuals with chronic pain were significantly higher compared to those that did not have chronic pain suggesting impaired functioning in the chronic pain cohort for the domains assessed. Further, all ASCQ-Me scores were significantly lower in individuals with chronic pain, also suggesting impaired pain and emotional functioning. Finally, painDETECT scores were significantly higher in patients with chronic pain, suggesting that neuropathic pain may be more likely to exist in those with chronic pain.
PROs are significantly worse in adults with SCD who have chronic pain as compared to those who do not have chronic pain, indicating substantially impaired functioning associated with chronic pain in multiple domains and highlighting the need for multidisciplinary care for chronic pain. Neuropathic pain also appears to be more prevalent in those with chronic pain suggesting targeted treatment for this type of pain may improve patient functioning. Future work is needed to validate the use of PROs as chronic pain assessment tools.
Disclosures
Hankins:ASH: Membership on an entity's Board of Directors or advisory committees; HRSA: Research Funding; CDC: Research Funding; NHLBI: Membership on an entity's Board of Directors or advisory committees, Research Funding; CVS Health: Consultancy; Forma Therapeutics: Consultancy; GBT: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.